This is a year and half old but I thought I'd throw it out there for the group -
https://www.fiercebiotech.com/research/could-astrazeneca-s-ovarian-cancer-drug-also-treat-glioblastoma
Pages
▼
Monday, 29 July 2019
Wednesday, 24 July 2019
A KETOGENIC PILL FOR GLIOBLASTOMA ?
Came across this study and would love to know others' thoughts. I have been following the progress of the ketogenic (almost no carbohydrate) diet for some time and its potential value in glioblastoma and epilepsy. This study seems to show that some of the purported benefits could be achieved through a ketone ester supplement, which serves to provide the brain with its alternative non-glucose fuel source (Ketone bodies)
direct link to abstract: https://academic.oup.com/neuro-oncology/article-abstract/20/suppl_6/vi36/5154383?redirectedFrom=fulltext )
Any thoughts on this, and how it might be translated to human use?
Thanks!
direct link to abstract: https://academic.oup.com/neuro-oncology/article-abstract/20/suppl_6/vi36/5154383?redirectedFrom=fulltext )
Any thoughts on this, and how it might be translated to human use?
Thanks!
Alternative to Bosellia Wokvel?
I've seen previous posts explaining the rationale behind the recommendation of Boswellia (WokVel) preparation. However, this formulation is currently out of stock from all suppliers in my area (UK). I note from Ben Williams' book that the dose of boswellia used in the cited German trial (showing reduced oedema) was 4200 mg/day, which is much higher than the 999mg suggested on this site. What's the best alternative to WokVel, given that I am unable to source it? I assume that taking it alongside Celecoxib is tried-and-tested?
Monday, 22 July 2019
Do statins, ACE inhibitors or sartans improve outcome in primary glioblastoma?
Hello all,
I spotted this paper and thought it was best to share: “Do statins, ACE inhibitors or sartans improve outcome in primary glioblastoma?” Although I’ve not read the full paper, it’s worth noting that they concluded:
I spotted this paper and thought it was best to share: “Do statins, ACE inhibitors or sartans improve outcome in primary glioblastoma?” Although I’ve not read the full paper, it’s worth noting that they concluded:
This secondary analysis of two large glioblastoma trials thus was unable to detect evidence for an association of the use of statins, ACEI or sartans with outcome in patients with newly diagnosed glioblastomaShould we abandon ACE inhibitors, etc?
Seeing feedback on proposed treatment plan and drug/ supplement cocktail
Hi Stephen,
I finally have medical data back for my dad and we had our first meeting with his oncology teams yesterday. I have summarized his medical data as well as our treatment plan below.
A couple of notes and questions upfront:
-
I didn't see anything on my dad's medical records about MGMT
-
Would greatly appreciate your feedback on the proposed drug cocktail and supplements
-
Are we missing anything?/ Dosages?
-
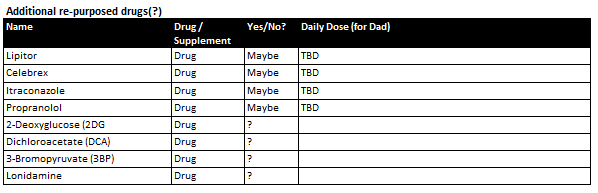
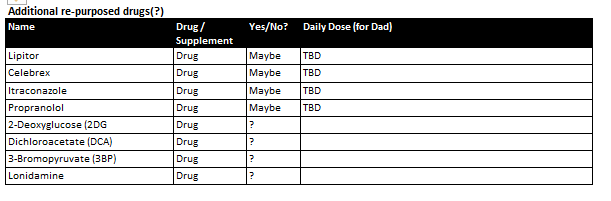
I would like to supplement COC protocol with some additional re-purposed drugs (particularly the first 4 in the table below. Do you have any information on dosage and how others go about getting prescriptions for these?
-
Many thanks again for your continued help.
Silvia
MEDICAL DATA:
-
Clinical synopsis
-
64M p/w expressive dyphasia and headache with likely malignant transformation of L) temporal LGG
-
2018 June generalised seizure diagnosed with left temporal mass likely LGG
-
Monitored as outpatient
-
Started on keppra and phenytoin for seizure control (self ceased keppra in
 January due to rash)
January due to rash)
-
Last seizure in April
-
July 2019 clinical synopsis
-
Presented with headaches and expressive dyphasia
-
Treatment
-
Stereotactic left temporal craniotomy and debulking of glioma (3 July)
-
Good postoperative course
-
Discharged 11 July
-
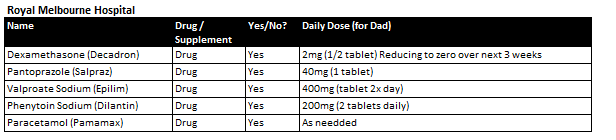
Medications
-
Histopathology results
-
Final Diagnosis: Left insula lesion: Glioblastoma. Features in keeping with IDH wild type (WHO grade IV)
-
GFAP positive
-
IDH-1 R132H negative (not mutated)
-
ATRX positive (not mutated)
-
P53 positive
-
P16 CDKN2A negative
-
Topoisomerase - approximately 20%
-
Post operative MRI
-
Small focus of residual enhancing tumour at the posterosuperior resection margin. Extensive oedema with midline shift measuring 9mm to the right and left uncal herniation has slightly improved
-
Recommending SOC treatment
-
Radiation / chemo to begin in ~3 weeks (~12 August)
-
Combined radiation & TMZ
-
Confirming targeted cavity and margin, not whole brain
-
Starting with 3 week course as patient is over 60
-
If patient is fit will recommend more aggressive 6 week treatment (TBD)
-
Followed by TMZ maintenance schedule
OUR CURRENT PLAN
-
Commence SOC protocol as prescribed by medical team in ~3 weeks
-
Complement with
-
(1) Ketogenic Diet
-
Strict 4:1 ratio, targeting Glucose / Ketone Index of 1:2 or lower (ideally 1:1 at 3mmol/ L each)
-
Calorie restricted ~900kcal/ day
-
Intermittent fasting (work towards target 2 - 8pm eating window)
-
Supplemented with Exogenous ketones (Caprilic acid and BHB salts during fasting window and can also be consumed during eating window)
-
(2) Repurposed drugs cocktail per Care Oncology Clinic (submitted info, waiting for treatment plan)
-

-
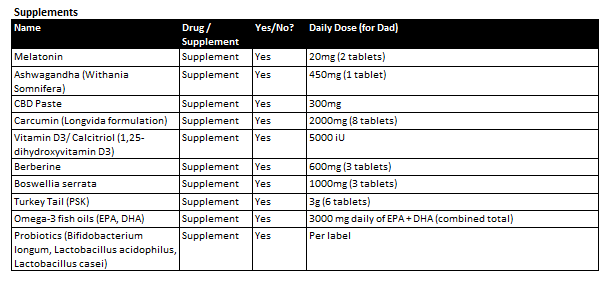
(3) Supplements
-
I didn't see anything on my dad's medical records about MGMT
Would greatly appreciate your feedback on the proposed drug cocktail and supplements
- Are we missing anything?/ Dosages?
- I would like to supplement COC protocol with some additional re-purposed drugs (particularly the first 4 in the table below. Do you have any information on dosage and how others go about getting prescriptions for these?
Clinical synopsis
- 64M p/w expressive dyphasia and headache with likely malignant transformation of L) temporal LGG
- 2018 June generalised seizure diagnosed with left temporal mass likely LGG
- Monitored as outpatient
- Started on keppra and phenytoin for seizure control (self ceased keppra in
January due to rash)
- Last seizure in April
- July 2019 clinical synopsis
- Presented with headaches and expressive dyphasia
- Treatment
- Stereotactic left temporal craniotomy and debulking of glioma (3 July)
- Good postoperative course
- Discharged 11 July
- Medications
Histopathology results
- Final Diagnosis: Left insula lesion: Glioblastoma. Features in keeping with IDH wild type (WHO grade IV)
- GFAP positive
- IDH-1 R132H negative (not mutated)
- ATRX positive (not mutated)
- P53 positive
- P16 CDKN2A negative
- Topoisomerase - approximately 20%
Post operative MRI
- Small focus of residual enhancing tumour at the posterosuperior resection margin. Extensive oedema with midline shift measuring 9mm to the right and left uncal herniation has slightly improved
Recommending SOC treatment
- Radiation / chemo to begin in ~3 weeks (~12 August)
- Combined radiation & TMZ
- Confirming targeted cavity and margin, not whole brain
- Starting with 3 week course as patient is over 60
- If patient is fit will recommend more aggressive 6 week treatment (TBD)
- Followed by TMZ maintenance schedule
Commence SOC protocol as prescribed by medical team in ~3 weeks
Complement with
- (1) Ketogenic Diet
- Strict 4:1 ratio, targeting Glucose / Ketone Index of 1:2 or lower (ideally 1:1 at 3mmol/ L each)
- Calorie restricted ~900kcal/ day
- Intermittent fasting (work towards target 2 - 8pm eating window)
- Supplemented with Exogenous ketones (Caprilic acid and BHB salts during fasting window and can also be consumed during eating window)
- (2) Repurposed drugs cocktail per Care Oncology Clinic (submitted info, waiting for treatment plan)
- (3) Supplements
Sunday, 21 July 2019
Curcumin preparation type?
Apologies if this is going over some issues previously discussed: There are lots of different curcumin pills and potions around, and 1000-2000 mg+ (Longvida) has been recommended elsewhere on this site. There seems to be a world of difference in how much curcumin gets into the brain depending on in what form it is taken.
I wondered on what basis is Longvida's product recommended? I noticed this 2015 conference presentation: "Intratumoral bioavailability and changes in Phosphoethanolamin-MRI of the solubilised natural compound curcumin in glioblastoma patients", which demonstrated how curcumin accumulated in glioblastoma tumours when it was given orally as "solubilisated curcumin". With a bit of internet searching using the terms in this study description, it seems to be that they used NovaSOL curcumin, or something very similar ("Micelle solubilized curcuma extract") I'm not sure how the doses used in the study (apparently a total of 3g of solubilized curcumin per day, which sounds like a heck of a lot!) equates to the NovaSOL capsules that can be bought (each of which contains just '30mg Curcuminoids and 5.4μg Vitamin D' ). Less certain again is how this might equate to an actual clinical effect on the tumour when combined with chemotherapy, although the likes of review articles such as 'Curcumin for the Treatment of Glioblastoma' would say that it is definitely worthwhile adding to the mix.
All input greatly received from cocktail-makers!
Thanks,
Stu
Stu
Saturday, 20 July 2019
Nicotine and brain tumour growth
Has the topic of nicotine (and other stimulants) been considered by the collective community?
My grade 2 astrocytoma was recently found to have advanced to grade 3(after 11years). Now IDH mutant, 1p / 19q not-codeleted, MGMT methylated. Both nicotine (via lozenges) and coffee are helpful in fighting fatigue and helping concentration.
Any thoughts? I am naturally concerned about taking anything that may hinder radiotherapy and chemotherapy (due to start at the beginning of August).
Thanks!
Stu
My grade 2 astrocytoma was recently found to have advanced to grade 3(after 11years). Now IDH mutant, 1p / 19q not-codeleted, MGMT methylated. Both nicotine (via lozenges) and coffee are helpful in fighting fatigue and helping concentration.
Any thoughts? I am naturally concerned about taking anything that may hinder radiotherapy and chemotherapy (due to start at the beginning of August).
Thanks!
Stu
Monday, 15 July 2019
IDH1+ GBM recurrence--any help appreciated!
Hi, I have found Stephen and many of you to be great sources of information over the years and would really appreciate any help. (Unfortunately, I can post but not comment thru some weird glitch.) I have given my son's background before, but briefly he is a 26 y/o with secondary GBM (IDH1+) which was found to have recurred on a scan today. He was diagnosed with AO2 (or perhaps AA3) in 2011 and had not quite total resection, "left-over" resected in 2012 and then had proton therapy as part of a clinical trial. He did well for over 5 years--graduated from college and started med school. He had a very small recurrence found 1/18 that had mutated to GBM (hypomutated with no actionable mutations other than IDH1 per Foundation One) with a very total resection. He had never had any chemo and we opted to use a PARP inhibitor (BGB-290) with temozolamide--started 4/18. He returned to medical school on chemo--tolerated both pretty well. Today found out that 3 mm area of "uncertain significance" found 7 weeks ago is now 2.6x2x2.7 cm and near a ventricle (though some of size likely incorporates scar). So, trying to figure out the next step.
He was offered TMZ and radiation as options. He wants to have the tumor "debulked", which seems supported in the medical literature. (His tumor is left frontal lobe.)
Options we have considered: TOCA (thru IST program maybe?) with proton
LITT with pembro
AZD-1390 trial --since ATM/ATR inhibitors useful if IDH1?
Duke Poliovirus--only works 21% and no better if mutant
(Of course, I don't know if he will qualify for any of these.)
Would very much appreciate any suggestions! Marcia
He was offered TMZ and radiation as options. He wants to have the tumor "debulked", which seems supported in the medical literature. (His tumor is left frontal lobe.)
Options we have considered: TOCA (thru IST program maybe?) with proton
LITT with pembro
AZD-1390 trial --since ATM/ATR inhibitors useful if IDH1?
Duke Poliovirus--only works 21% and no better if mutant
(Of course, I don't know if he will qualify for any of these.)
Would very much appreciate any suggestions! Marcia
Newly Diagnosed GBM
Hi all,
My name is Silvia, I am new to this community and a week ago knew nothing about GBM. I'm incredibly grateful for the wealth of information here and would like to thank everyone in advance for your support.
My 64 father was diagnosed with glioblastoma last week. He had a subtotal resection on July 3rd which was successful in removing ~95% of the solid part of his tumor. He is recovering well and was discharged from hospital on July 11th.
My 64 father was diagnosed with glioblastoma last week. He had a subtotal resection on July 3rd which was successful in removing ~95% of the solid part of his tumor. He is recovering well and was discharged from hospital on July 11th.
He is based in
Melbourne Australia and is being treated by the team at Royal Melbourne
Hospital, who are recommending the radiation/TMZ protocol. I am still
waiting for them to send me his medical data but our current plan is the
following
- Press-Pulse
protocol as a
neoadjuvant treatment while he is recovering from surgery with the hope
that if there is improvement in his MRI we can delay chemo/radiation
- Details of the protocol:
- Based off the metabolic
theory of cancer
- Press (ongoing):
- Ketogenic Diet with
intermittent fasting supplemented with exogenous ketones
- Low dose metformin
- Pulse:
- Hyperbaric Oxygen
therapy
- High dose IV vitamin C
- Cancer
specific glycolytic inhibitors: (e.g. 2-Deoxyglucose (2DG),
Dichloroacetate (DCA), 3-Bromopyruvate (3BP); Lonidamine)
- insulin
potentiation
- https://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-017-0178-2
- https://peterattiamd.com/domdagostino/ [Dom
describes the protocol for GBM at 1:59:45]
- https://www.frontiersin.org/articles/10.3389/fnut.2018.00020/full
- Repurposed Drug/ Supplement
cocktail
- Will post details of this to
get feedback once I have his detailed diagnosis and a consultation with
the Care Oncology Clinic
- Proceed with radiation/ chemo
if no improvement in MRI prior to planned start date
I have a few questions
for now:
- Has anyone in this community tried the press-pulse protocol and if so how (what parts, neoadjuvant/ concurrent/ adjuvant with SOC etc.?) and with what result? Does anyone know of any practitioners located in Australia that might be able to help in implementing the protocol?
- Has anyone had any experience
with the Burzynski clinic / Antineoplastons? (https://www.burzynskiclinic.com/)
·
For context: My mum
and dad are very against radiation and chemo, and unfortunately subscribe to
big pharma conspiracy theories. They are searching for information on youtube
which means that on top of the research I am doing myself, I must also spend a
lot of time researching and more often than not debunking the “cures” they come
across
·
The quick research
I've done on this seems to suggest it's controversial and unproven
- Does anyone know if there is any harm with Laetrile (Vitamin B17 /Amygdalin)? I know there is no evidence to support its efficacy but my mum is convinced it will help and I wonder if its worth fighting her on it if it doesn't do any harm (she's currently giving him apricot kernels ~ 40-50 / day)
- Similarly with Phour Salts?
Thank you all in advance for any information you might be able to share!
Silvia
Saturday, 13 July 2019
Question About D-Dimer Blood Test
Hello All,
Does anyone have good knowledge on D-Dimer and its importance? I understand that there can sometimes be false positives on results, but if a D-Dimer reading came back super high should the patient go in for a scan right away for clots? The range is .20-.45, my Uncle's just came back at 2.25. Any advice appreciated.
Thank You ~
Does anyone have good knowledge on D-Dimer and its importance? I understand that there can sometimes be false positives on results, but if a D-Dimer reading came back super high should the patient go in for a scan right away for clots? The range is .20-.45, my Uncle's just came back at 2.25. Any advice appreciated.
Thank You ~
Tuesday, 9 July 2019
Antioxidant use in IDH1 mutant tumors
I'd like to open a topic up for debate here regarding antioxidant use in IDH1 mutant tumors. My understanding is that IDH1 mutant tumors are characterized by generally low Glutathione (antioxidant) levels, significantly sensitizing them to ROS generation. Some researchers speculate that this is the primary reason for superior OS stats for IDH1 mutant tumors, e.g.:
Given this particular dynamic, should I conclude that use of antioxidants which stimulate Glutathione (e.g. Alpha Lipoic Acid, Green tea, Cinnamon,...) should better be avoided in the case of IDH1 mutant tumors?
I am particularly interested in this question as my tumor is IDH1 mutated, and I recently started taking the Metabloc protocol (Alpha Lipoic Acid + Hydroxycitrate), since it seems to deliver very promising synergy with Metformin use. After investigating a bit, I am contemplating skipping the Alpha Lipoic Acid, however.
Any thoughts on this topic? Thanks!
John