Hi everyone,
Few questions regarding my mother, who unfortunately has had a recurrence of her Glioblastoma.
BACKGROUND
In August 2019, the Neurological Institute of McGill University (Montreal, Canada) discovered the tumor. My mother had a full resection in September 2019. Pathology : Glioblastoma grade 4, IDH1 wild type - MGMT unmethylated.
After the surgery, the Neuro team has put her on their M-HARTT STUDY https://clinicaltrials.gov/ct2/show/NCT02780024 - which means having condensed radiotherapy (4 weeks) with TMZ, then TMZ for 6 months and Metformin (850) on a daily basis.
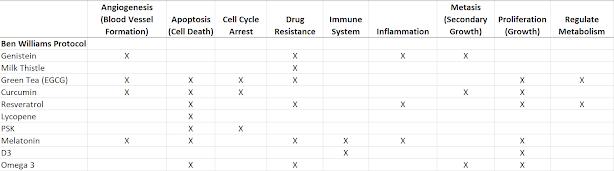
My mother and myself have been very inspired by Ben Williams, this blog, the Surviving Terminal Cancer documentary and Stephen/Ben Williams documents https://virtualtrials.com/pdf2017/treatment_options_gbm_2017.pdf
We've added repurposed drugs and supplements to her diet, which I've listed below.
My mother recovered well from the operation of September 2019, being back to her 100% during the summer and having a clean MRI in July.
Her MRI of September showed a mass of 2.5cm appeared in her brain. Neither the neurosurgeon, nor the oncologist knew whether it was radio-necrosis or a recurrence. We decided to wait for a month to see how it progressed, adding 4mg decadron to her medications. October 2020, the mass had grown 8mm, so we decided to go into surgery.
My mother was operated 2 days ago, the surgery was done using 5-aminolevulinic acid (ALA) - which has only very recently been approved in Canada. She's well recovered from it thus far, she's still in the hospital. It seems they've removed most of the tumor, although the 5-ALA technology showed there were small cancer cells left.
We're currently waiting for the pathology from the lab and we'll also send the tumor to Foundation One. I know the results from both these analysis will guide us for the next steps, but I wanted to turn to this blog community - which I highly respect and estimate - to get all the knowledge to navigate through the next steps for this fight against GBM.
Here are my questions:
1) What are the treatment options for this first recurrence and which one would you recommend?
2) Are there specific questions I should ask regarding the pathology and the results from Foundation One ?
3) From the list of repurpused drugs below, any of them you'd recommend we cut out or we add ?
4) Do you think CUSP9 would be appropriated in this situation and/or any other repurposed drugs?
5) Would it be a good idea to consider Ben William's approach to chemo, i.e. BCNU chemotherapy with tamoxifen, verapamil, Accutane ?
LIST OF MEDICATIONS AND SUPPLEMENTS
- Temozolomide (from Octobre 2019 to May 2020)
- Celebrex (from October 2019 until now)
- Melatonin (from October 2019 until now)
- Vitamin D (from October 2019 until now)
- Metformin (from October 2019 until now)
- Keppra (from October 2019 until now)
- Pantoprazole (from October 2019 until now)
- Atorvastatin (Summer 2020 until now)
- Silibinin extract (Spring 2020 until now)
- Selenium (Spring 2020 until now)
- Omega-3 Fish Oil Extract (Spring 2020 until now)
- Coriolus versicolor extract PSK (Spring 2020 until now)
- Curcumin with Peper - longvida (Spring 2020 until now)
- Maitake-D mushroom extract (Spring 2020 until now)
- Reishi mushroom extract (Spring 2020 until now)
- Green Tea Extract (Spring 2020 until now)
- Soy Isoflavones (Spring 2020 until now)
- Resveratrol (Spring 2020 until now)
- Boswellia Serrata (September 2020 until now)
- Tumeric with peper (October 2019 until now)
- Green Tea (October 2019 until now)
Many thanks for taking the time to read this,
Bertrand
P.S. For the French speakers/Canadians out there, there was a Radio-Canada (CBC) news piece about McGill's research for a new treatment against GBM - the ZR2002 molecule - where my mother was featured (we've been encouraging their research):
https://ici.radio-canada.ca/nouvelle/1469050/maladie-orpheline-meurtriere-interesse-pharmaceutiques
https://pubmed.ncbi.nlm.nih.gov/31540977/