My husband developed permanent pill fatigue a few months ago and I have the following supplements/meds to give away. Many are sealed, but a few are open so specify which you would like and whether you feel comfortable with open bottles. I prefer they go to someone who is under financial strain. I am happy to send to the first couple of people who respond with their mailing addresses.
Wishing you all a peaceful holiday season! Sharon
Life Extension Super R-Lipoic Acid 240 mg
Panacur C (Fenbendazole)
Hydroxycitrate--Solgar
Zinc 50 mg--Life Extension--opened and sealed
Shark Liver Oil 500 mg-- Solgar
Optimized Resveratol Life Extension--opened
EGCg 400 mg NOW
Mushroom Science Turkey Tail Coriolus Super Strength
Kyolic (Aged Garlic Extract/Lecithin)
Lycopene 10 mg--Puritan's Pride--opened
Sunflower Lecithin 1200 mg Softgels Now--opened
Optimized Curcumin 1000 mg Longvida --opened
Berberine 500 mg--Amazing Formulas
Melatonin 10 mg-- Nature's Best
Tuesday, 24 December 2019
Monday, 23 December 2019
Hi all and Merry Christmas,
My 23yo son was diagnosed with a Diffuse Astrocytoma, right frontal lobe. Had an awake craniotomy on Oct 15. According to Dec 6, MRI some may have been left behind due to location at/near motor cortex but surgeon also says could be inflammation or scar tissue. Recommends starting 6 weeks radiation in January, followed by 1 year of chemo (Temodar). Wondering if anyone has ever delayed treatment. Also, what supplements would you advise? Do you take them during treatment? I have searched through other posts but want to make sure I do the right thing according to his pathology report. Thank you so much for your help!
Anatomic Pathology Diagnosis:
IDH-mutant, WHO 2016 grade II
IDH1 R132H positive
ATRX expression with focal loss
1p/19q NOT deleted
Molecular Diagnostics Results:
79 Gene Mutation Analysis - 1 Mutation Detected
IDH1:ENST00000415913.1:c.395G>A; p.Arg132His
TP53:ENST00000269305.4:c.818G>A; p.Arg273His
CDKN2B:ENST00000276925.6c.367C>T; p.Arg123Trp
PTEN deletion DETECTED
TERT gene promoter mutation NOT detected
MGMT promoter methylation NOT detected
EGFR gene NOT amplified
Tuesday, 3 December 2019
Hi everyone!
My 14 year old son, Eli, has recurrent, metastatic medulloblastoma. The disease is in his bone marrow and bones.
He was first diagnosed in May 2017. He had a resection, 30 rounds of radiation and 7 cycles of chemo (cyclophosphamide, vincristine, cisplatin, premextred and gemcitabine). Eli had no evidence of disease for 2 years.
His recurrence was diagnosed September 2019. He had 2 cycles of temozolomide, irinotecan and avastin before this was stopped due to progression. His CNS remains clear of disease with only bone and bone marrow involvement.
I am now trying to decide between 2 different treatment options. 1) ACT001 (otherwise known as parthenolide). This would be a stand alone treatment that has mixed responses from adult glioblastoma patients. 2) A new trial called SJELIOT which consists of either cyclophosphamide and prexasertib (CHEK1/CHEK2 inhibitor) or gemcitabine and prexasertib. This is a new trial targeted at relapse medulloblastoma.
I am also in touch with Care Oncology Clinic in London but due to Eli's age they can only advise and cannot take him on as a patient.
Does anyone have any advice for me please?
My 14 year old son, Eli, has recurrent, metastatic medulloblastoma. The disease is in his bone marrow and bones.
He was first diagnosed in May 2017. He had a resection, 30 rounds of radiation and 7 cycles of chemo (cyclophosphamide, vincristine, cisplatin, premextred and gemcitabine). Eli had no evidence of disease for 2 years.
His recurrence was diagnosed September 2019. He had 2 cycles of temozolomide, irinotecan and avastin before this was stopped due to progression. His CNS remains clear of disease with only bone and bone marrow involvement.
I am now trying to decide between 2 different treatment options. 1) ACT001 (otherwise known as parthenolide). This would be a stand alone treatment that has mixed responses from adult glioblastoma patients. 2) A new trial called SJELIOT which consists of either cyclophosphamide and prexasertib (CHEK1/CHEK2 inhibitor) or gemcitabine and prexasertib. This is a new trial targeted at relapse medulloblastoma.
I am also in touch with Care Oncology Clinic in London but due to Eli's age they can only advise and cannot take him on as a patient.
Does anyone have any advice for me please?
Thursday, 28 November 2019
HAART Antivirals? Atorvastatin dosage?
My dad is on valtrex (valaciclovir/valacyclovir) daily and I noticed it is a guanosine analogue. I was wondering if anyone is taking HIV HAART treatment, such as tenofovir as well? It is a adenosine analogue and therefore I would imagine would work well to bind to Cytosine and Valtrex to Thymine in the cancer DNA? I would imagine antiviral drugs are limited if only 1 of 4 potential DNA base analogues is used? I know the CUSP9 protocol is using ritonavir but it is just used by itself - perhaps a cocktail of antivirals need to be used to combine with the cancer DNA?
Also we were wondering about Atorvastatin dosage as he is on 20mg a day but Care Oncology seem to recommend people are on 80mg a day? Do people get side effects on this dosage? Should we increase the dosage?
Background on my dad:
My father was diagnosed with Grade 4 GBM after a grand mal seizure 24th Feb 2019. Located in the left temporal lobe.
He had a successful craniotomy on the 7th of March 2019
He completed the 30 sessions and then 3 months of 5/23 TMZ chemo. In September 2019, there was alot of swelling/looked like the tumor was very active by MRI and due to MGMT unmethylation the hospital stopped the TMZ and have now been giving him Avastin on Mondays every 2 weeks. Bloods are all normal and within range.
He was having trouble with speach and twitching in September time but this is now gone and he is back to 100% after adding Phenytoin, Clobazam and Dexamethasone
He was having trouble with speach and twitching in September time but this is now gone and he is back to 100% after adding Phenytoin, Clobazam and Dexamethasone
Daily:
Seizure drugs: 1.5g x 2 Keppra ; Phenytoin; clobazam daily.
He carries around Midazolam injections in case he was ever to have a seizure but has only had 2 occassions this year.
He carries around Midazolam injections in case he was ever to have a seizure but has only had 2 occassions this year.
2 x 2 mg Dexamethasone daily
Experimental Drug Cocktail (Ben Williams):
1g x 2 Valtrex (valaciclovir/valacyclovir); Chloroquine (155mg active ingredient); Celebrex 200mg; metformin 500mg x 2; 20mg Atorvastatin; ramipril; ranitidine 75 mg; melatonin 20mg; 100mg mebendazole (1 month on/1 month off); 100 mg x 2 minocycline (1 month on/1 month off);
Daily supplements of multivitamin; 16 strain Probiotics; PSK; Maitake D; ; Mushroom supplement mix for brain (lions mane 300mg; bacopa 250 mg; reishi 150 mg; gotu kola 130 mg; ginko 120 mg); curcumin (longvida); vitamin D; ECG; Milk Thistle; Berberine; Boswellia; Resveratrol; Omega 3-6-9; Soy Falvonoids (geinistein); Astragalus; Artemisinin
Labels:
atorvastatin,
chloroquine,
HAART,
keppra_levetiracetam,
mebendazole,
melatonin,
metformin,
MGMT_unmethylated,
minocycline,
ramipril,
ranitidine,
ritonavir,
valtrex_valacyclovir_valaciclovir
Wednesday, 27 November 2019
Avastin or Lomustine to prioritize?
Hi, those of you who are on combined Avastin + Lomustine for recurrence and struggling with blood counts, what is your experience, which treatment your oncologist prioritizes in need?
My husband who is a 32 months survivor with multifocal GBM progressed during his 2nd radiotherapy and his doctor gave up on him stating that he had less than 1 month of life expectancy. But luckily he reacted well to Avastin and his serious symptoms disappeared within days after the 1st infusion.
Together with the 2nd infusion we added lomustine (90 mg / m2) and it messed up with his blood counts on week 4 and 6 so his oncologist postponed both treatments. Plus, a few days after the combination treatment he started having severe diarrhea that is still ongoing and it didn't improve on those 2 weeks when we paused Avastin. He became weaker and weaker gradually.
Shortly after finally receiving the 4th Avastin with delay, he ended up in the ER due to confusion and seizures that we didn't experience in the past 3 months at all. Seizures were the first signs of tumor progression back in April so now we're frightened. Methylprednisolone was doubled to 64 mg (equivalent of 13 mg dex), Keppra was increased to 3000 mg. Symptoms disappeared within 2 days. Emergency CT showed only a very slight swelling which is actually an improvement compared to the last MRI in late August.
Today we were on pins and needles to finally start the 2nd cycle of Lomustine (we're already in more than 2 weeks delay) after his blood work results came back as perfect (BP 220,000, WBC 6.8) but the oncologist advised "Don't risk Avastin."
Avastin is a palliative treatment while chemo can really help if someone has a good reaction to it (TMZ helped him for 2 years) so I don't understand why the oncologist put Lomustine on hold in favor of Avastin considering that it is very likely that the tumors are progressing again? What's the point in using Avastin if he still needs tremendous amounts of steroids, plus he lays in bed most of the day despite the treatment? Next MRI will be in early December.
By the way, we sourced Lomustine from India because the oncologist wasn't able to prescribe it due to local protocols. He is only allowed to prescribe it after the failure of Avastin so we're actually not depending on his decision, it's just not a wise thing to disagree with your doctor.
My main concern is that there's some evidence that no chemo is able to help after the failure of Avastin so I can't see the reason why to wait for further progression in order to continue Lomustine, providing that his blood counts are perfect at the moment.
Thank you for any advice that you can provide.
My husband who is a 32 months survivor with multifocal GBM progressed during his 2nd radiotherapy and his doctor gave up on him stating that he had less than 1 month of life expectancy. But luckily he reacted well to Avastin and his serious symptoms disappeared within days after the 1st infusion.
Together with the 2nd infusion we added lomustine (90 mg / m2) and it messed up with his blood counts on week 4 and 6 so his oncologist postponed both treatments. Plus, a few days after the combination treatment he started having severe diarrhea that is still ongoing and it didn't improve on those 2 weeks when we paused Avastin. He became weaker and weaker gradually.
Shortly after finally receiving the 4th Avastin with delay, he ended up in the ER due to confusion and seizures that we didn't experience in the past 3 months at all. Seizures were the first signs of tumor progression back in April so now we're frightened. Methylprednisolone was doubled to 64 mg (equivalent of 13 mg dex), Keppra was increased to 3000 mg. Symptoms disappeared within 2 days. Emergency CT showed only a very slight swelling which is actually an improvement compared to the last MRI in late August.
Today we were on pins and needles to finally start the 2nd cycle of Lomustine (we're already in more than 2 weeks delay) after his blood work results came back as perfect (BP 220,000, WBC 6.8) but the oncologist advised "Don't risk Avastin."
Avastin is a palliative treatment while chemo can really help if someone has a good reaction to it (TMZ helped him for 2 years) so I don't understand why the oncologist put Lomustine on hold in favor of Avastin considering that it is very likely that the tumors are progressing again? What's the point in using Avastin if he still needs tremendous amounts of steroids, plus he lays in bed most of the day despite the treatment? Next MRI will be in early December.
By the way, we sourced Lomustine from India because the oncologist wasn't able to prescribe it due to local protocols. He is only allowed to prescribe it after the failure of Avastin so we're actually not depending on his decision, it's just not a wise thing to disagree with your doctor.
My main concern is that there's some evidence that no chemo is able to help after the failure of Avastin so I can't see the reason why to wait for further progression in order to continue Lomustine, providing that his blood counts are perfect at the moment.
Thank you for any advice that you can provide.
Saturday, 23 November 2019
Low dose perampanel added to levetiracetam (Keppra)
Experience of Low Dose Perampanel to Add-on in Glioma Patients with Levetiracetam-uncontrollable Epilepsy
Abstract
After introduction of levetiracetam (LEV), treatment of seizures in patients with malignant brain tumors has prominently improved. On the other hand, we still experience some cases with LEV-uncontrollable epilepsy. Perampanel (PER) is a noncompetitive α-amino-3-hydroxy-5-methyl-4-isoaxazolepropionate acid receptor antagonist that has recently been approved for treating focal epilepsy as a secondary drug of choice. Available literature reporting PER medication in patients with gliomas is still sparse. Here, we report our initial experience with glioma patients and report efficacy of adding low dose 2-4 mg PER to LEV in patients whose seizure were uncontrollable with LEV monotherapy. Clinical outcome data of 18 consecutive patients were reviewed. This included nine males and nine females aged 24-76 years (median, 48.5 years), treated for glioma between June 2009 to December 2018. We added PER to patients with LEV-uncontrollable epilepsy. Adverse effects, irritability occurred in two patients, but continuous administration was possible in all cases. Though epileptic seizures occurred in four cases receiving 2 mg PER, 17 cases achieved seizure freedom by dose increments; final dose, 2-4 mg PER added to LEV 500-3000 mg. Our study revealed anti-epileptic efficacy of low dose PER 2-4 mg as first add-on therapy to LEV in glioma patients who have failed or intolerable to LEV monotherapy. Low dose PER added on to LEV may have favorable efficacy with tolerable adverse effects in glioma patients with LEV-uncontrollable epilepsy.
https://www.ncbi.nlm.nih.gov/pubmed/31748440
Abstract
After introduction of levetiracetam (LEV), treatment of seizures in patients with malignant brain tumors has prominently improved. On the other hand, we still experience some cases with LEV-uncontrollable epilepsy. Perampanel (PER) is a noncompetitive α-amino-3-hydroxy-5-methyl-4-isoaxazolepropionate acid receptor antagonist that has recently been approved for treating focal epilepsy as a secondary drug of choice. Available literature reporting PER medication in patients with gliomas is still sparse. Here, we report our initial experience with glioma patients and report efficacy of adding low dose 2-4 mg PER to LEV in patients whose seizure were uncontrollable with LEV monotherapy. Clinical outcome data of 18 consecutive patients were reviewed. This included nine males and nine females aged 24-76 years (median, 48.5 years), treated for glioma between June 2009 to December 2018. We added PER to patients with LEV-uncontrollable epilepsy. Adverse effects, irritability occurred in two patients, but continuous administration was possible in all cases. Though epileptic seizures occurred in four cases receiving 2 mg PER, 17 cases achieved seizure freedom by dose increments; final dose, 2-4 mg PER added to LEV 500-3000 mg. Our study revealed anti-epileptic efficacy of low dose PER 2-4 mg as first add-on therapy to LEV in glioma patients who have failed or intolerable to LEV monotherapy. Low dose PER added on to LEV may have favorable efficacy with tolerable adverse effects in glioma patients with LEV-uncontrollable epilepsy.
https://www.ncbi.nlm.nih.gov/pubmed/31748440
Friday, 22 November 2019
Good day to all!
Maybe Stephen or some of the blog readers will be able to comment. I will be very grateful.
Two months ago my sister had a second operation (I wrote about this on this blog a while ago https://btcocktails.blogspot.com/2019/10/good-afternoon-stephen-and-all-thank.html), and in early November we did an MRI. The doctor said that the tumor did not grow, but there was perifocal edema, which is a consequence of radiation. Literally - "this is not the edema to be feared." He said that he could last up to a year and leave himself. According to the doctor, everything is normal. But she feels much worse than some time ago. She constantly sleeps, the left side of her body works worse (before the operation, neither her arm nor leg worked at all, and afterwards she got better), there is a squint. The symptoms are very similar just to the growth of edema, about the same as before the operation. We reduced dexamethasone after surgery and had already reached 24 mg to 3 mg, but yesterday the doctors decided to increase it to 4 mg.
Doctors also said that she had vestibulopathy (dizzy), salt in the ear. Low potassium. We started drinking Boswellia about a week ago to make it easier to leave dexamethasone, but somehow it did not help. But they took only 1 capsule (according to the instructions on the bank, 3 per day is needed), because we were told that it should also be added gradually. Maybe it was necessary to take 3 cupsules? Until recently, we did not want to raise dexamethasone again, and we are now very worried about the deterioration.
Tell me, please, is it really possible to leave dex in our situation and how to do it right? Raise the dose (which has already been done), stabilize the condition, and then again slowly reduce it (before, 0.5 mg per week was removed approximately)? How to remove / control edema?
Thank you in advance for responding!
Maybe Stephen or some of the blog readers will be able to comment. I will be very grateful.
Two months ago my sister had a second operation (I wrote about this on this blog a while ago https://btcocktails.blogspot.com/2019/10/good-afternoon-stephen-and-all-thank.html), and in early November we did an MRI. The doctor said that the tumor did not grow, but there was perifocal edema, which is a consequence of radiation. Literally - "this is not the edema to be feared." He said that he could last up to a year and leave himself. According to the doctor, everything is normal. But she feels much worse than some time ago. She constantly sleeps, the left side of her body works worse (before the operation, neither her arm nor leg worked at all, and afterwards she got better), there is a squint. The symptoms are very similar just to the growth of edema, about the same as before the operation. We reduced dexamethasone after surgery and had already reached 24 mg to 3 mg, but yesterday the doctors decided to increase it to 4 mg.
Doctors also said that she had vestibulopathy (dizzy), salt in the ear. Low potassium. We started drinking Boswellia about a week ago to make it easier to leave dexamethasone, but somehow it did not help. But they took only 1 capsule (according to the instructions on the bank, 3 per day is needed), because we were told that it should also be added gradually. Maybe it was necessary to take 3 cupsules? Until recently, we did not want to raise dexamethasone again, and we are now very worried about the deterioration.
Tell me, please, is it really possible to leave dex in our situation and how to do it right? Raise the dose (which has already been done), stabilize the condition, and then again slowly reduce it (before, 0.5 mg per week was removed approximately)? How to remove / control edema?
Thank you in advance for responding!
Monday, 18 November 2019
Tuesday, 29 October 2019
Hi, I write again seeking advice. I have very much appreciated comments/advice over the years and the expertise of those on this blog. Unfortunately, for some weird reason I cannot respond to responses, but am very appreciative!
My 26 y/o son has had another recurrence of his IDH1+ secondary GBM in L frontal lobe..
To summarize his past history, he had an AA3 diagnosed when he was 18 y/o treated with GTR and proton therapy only (clinical study) and had 5 good years where he graduated from college (with honors), worked and started medical school. His tumor recurred his 1st year of med school as a very small area of IDH1+ low mutation GBM (unmethylated) treated with aggressive GTR and then started on BGB-290 and TMZ study. He was on study from 4/18 thru 7/19. He completed a year of med school successfully while on chemo, but pretty low doses of TMZ used due to anemia (needed a few transfusions). A 3 mm "scar" seen on 5/19 scan grew into a large tumor by 7/19. So, since not great options, we opted for immunotherapy given his hematologic issues with preceding therapy--he was enrolled in IL-12 + Veledimex +PD1. His recurrent tumor was found to be hypermutated and now methylated (?)--so thought it turned out to be an appropriate choice. He had another GTR 8/19 with excellent neuro recovery. His MRI showed a strong inflammatory response around meninges/spinal cord, which study group felt was due to treatment (and they were correct). Anyway, MRI at 2 months after surgery showed a large L frontal lobe mass--thought was that it could be pseudoprogression, but surgical path showed all tumor (don't have final path yet).
So...he had another GTR (fabulous neurosurgeon) and has no obvious cognitive deficits (he is tutoring Latin grammar at the moment). He starts radiation next week (has been 7 years since proton) and will likely still have immunotherapy and ...something else. (Immunotherapy--likely Keytruda which is FDA-approved for mismatch repair deficient tumors?)
His current neuro-oncologist seems excellent, but the question is what else?
Options that have been considered--olaparib--radiosensitizing and might work with IDH1
--CCNU--old standby--don't know how long will tolerate
--regorafenib--superior to CCNU in one study--fewer blood probs?
Interestingly, his tumor did not grow at all in the 2 weeks before surgery, so wonder if immunotherapy was starting to kick in, though I was told that tumor growth is not always linear.
I know that this history is long and somewhat technical, but also that there are some very knowledgeable people on this blog. Any insights of those on immunotherapy, CCNU or regorafenib would be appreciated. I would also be curious if anyone has been on olaparib--it was tolerated well with radiation in elderly patients in British study.
Thank you so much for any help you can give....Anne
My 26 y/o son has had another recurrence of his IDH1+ secondary GBM in L frontal lobe..
To summarize his past history, he had an AA3 diagnosed when he was 18 y/o treated with GTR and proton therapy only (clinical study) and had 5 good years where he graduated from college (with honors), worked and started medical school. His tumor recurred his 1st year of med school as a very small area of IDH1+ low mutation GBM (unmethylated) treated with aggressive GTR and then started on BGB-290 and TMZ study. He was on study from 4/18 thru 7/19. He completed a year of med school successfully while on chemo, but pretty low doses of TMZ used due to anemia (needed a few transfusions). A 3 mm "scar" seen on 5/19 scan grew into a large tumor by 7/19. So, since not great options, we opted for immunotherapy given his hematologic issues with preceding therapy--he was enrolled in IL-12 + Veledimex +PD1. His recurrent tumor was found to be hypermutated and now methylated (?)--so thought it turned out to be an appropriate choice. He had another GTR 8/19 with excellent neuro recovery. His MRI showed a strong inflammatory response around meninges/spinal cord, which study group felt was due to treatment (and they were correct). Anyway, MRI at 2 months after surgery showed a large L frontal lobe mass--thought was that it could be pseudoprogression, but surgical path showed all tumor (don't have final path yet).
So...he had another GTR (fabulous neurosurgeon) and has no obvious cognitive deficits (he is tutoring Latin grammar at the moment). He starts radiation next week (has been 7 years since proton) and will likely still have immunotherapy and ...something else. (Immunotherapy--likely Keytruda which is FDA-approved for mismatch repair deficient tumors?)
His current neuro-oncologist seems excellent, but the question is what else?
Options that have been considered--olaparib--radiosensitizing and might work with IDH1
--CCNU--old standby--don't know how long will tolerate
--regorafenib--superior to CCNU in one study--fewer blood probs?
Interestingly, his tumor did not grow at all in the 2 weeks before surgery, so wonder if immunotherapy was starting to kick in, though I was told that tumor growth is not always linear.
I know that this history is long and somewhat technical, but also that there are some very knowledgeable people on this blog. Any insights of those on immunotherapy, CCNU or regorafenib would be appreciated. I would also be curious if anyone has been on olaparib--it was tolerated well with radiation in elderly patients in British study.
Thank you so much for any help you can give....Anne
Monday, 28 October 2019
A hopefully encouraging update
Hello all,
I hope to offer some feedback and encouragement to others on their brain tumour journey.
I have not long finished six and a half weeks' (33 fractions) radiotherapy with daily temozolomide. The first post-radiotherapy scan was far better than we could have hoped for. Although I have yet to see the scans, the oncologist said he was delighted and was struggling to see evidence of residual tumour (even though we understand that there was some left in the corpus callosum). He looked a little surprised, I might add. He is now rather more interested in the supplements I am taking than he was pre-radiotherapy!
My tumour: anaplastic astrocytoma right frontal lobe, WHO Grade III, MGMT methylated, IDH1 mutation positive, ATRX expression lost, p53 wild type, Ki-67 20-25%,
Supplements/Repurposed meds:
During radiotherapy I exercised 10-15 minutes twice a day on a bicycle rigged up to a turbo trainer.
Diet-wise: I tried to avoid big, carbohydrate-heavy meals, ate lots of nuts, seeds, eggs and fish, and salad/vegetables. My energy levels actually increased during the radiotherapy (!) (I think this may have been partly because I was still recovering from the surgery when the radiation started).
I would therefore say that the above regimen has stood me in good stead so far and happy to answer any questions on my experiences to date. I have just finished the first cycle of temozolomide (at a higher dose than that during radiotherapy).
I hope to offer some feedback and encouragement to others on their brain tumour journey.
I have not long finished six and a half weeks' (33 fractions) radiotherapy with daily temozolomide. The first post-radiotherapy scan was far better than we could have hoped for. Although I have yet to see the scans, the oncologist said he was delighted and was struggling to see evidence of residual tumour (even though we understand that there was some left in the corpus callosum). He looked a little surprised, I might add. He is now rather more interested in the supplements I am taking than he was pre-radiotherapy!
My tumour: anaplastic astrocytoma right frontal lobe, WHO Grade III, MGMT methylated, IDH1 mutation positive, ATRX expression lost, p53 wild type, Ki-67 20-25%,
Supplements/Repurposed meds:
Boswellia extract (WokVel)`
|
999mg / day
|
Etodolac
|
600mg
|
Omeprazole
|
20mg od
|
Curcumin (Longvida preparation)
|
1000-2000mg
|
CBD oil
|
50mg+/day
|
ECGC (green tea extract)
|
Teavigo preparation, 1/day
|
Melatonin
|
20 mg before bed
|
Omega-3 fish oils (EPA, DHA)
|
3000 mg daily of EPA + DHA
|
Selenium
|
200 mcg daily
|
Vitamin D3; or Alfacalcidol .(prescription)
|
5000-10,000 IU daily Vitamin D3
|
Chloroquine phosphate
|
250 mg daily;
|
During radiotherapy I exercised 10-15 minutes twice a day on a bicycle rigged up to a turbo trainer.
Diet-wise: I tried to avoid big, carbohydrate-heavy meals, ate lots of nuts, seeds, eggs and fish, and salad/vegetables. My energy levels actually increased during the radiotherapy (!) (I think this may have been partly because I was still recovering from the surgery when the radiation started).
I would therefore say that the above regimen has stood me in good stead so far and happy to answer any questions on my experiences to date. I have just finished the first cycle of temozolomide (at a higher dose than that during radiotherapy).
Musella yahoo groups shutting down. New forum address
Here is a message from Al Musella. Please check out and support his new forum.
This group is closing down as Yahoo no longer will provide groups. We are moving to forum.virtualtrials.org
Please register there and try it out!
Tuesday, 22 October 2019
Hi Stephen, hi all,
i read good things about the photodynamix therapy, for example:
https://www.ncbi.nlm.nih.gov/pubmed/25915500
One question about that topic does not let me go: Would it be possible to use that technique after a "full resection" or as an conservation thearapy when there is no tumor visible?
Don`t you think you could attack left over cells that way?
Thank you for an response!
All good!
i read good things about the photodynamix therapy, for example:
https://www.ncbi.nlm.nih.gov/pubmed/25915500
One question about that topic does not let me go: Would it be possible to use that technique after a "full resection" or as an conservation thearapy when there is no tumor visible?
Don`t you think you could attack left over cells that way?
Thank you for an response!
All good!
Wednesday, 16 October 2019
Good afternoon, Stephen and all!
Thank you so much for this blog, for the large amount of useful information that can be found here. This is very important for everyone who has faced such a terrible disease. We would like to tell you about our situation and we really look forward to your help, since we do not know at all what is best to do in our case. My sister (48 years old) was diagnosed with glioblastoma multiforme in April that affects affecting the insular lobe of the telencephalon and the right frontal lobe of the brain (IDH wild type; MGMT is unmethylated; ATRX obtained). At the moment, we do not have any other data on genetic mutations, a full genetic analysis will be available only after 3 weeks. 4 days after diagnosis, an operation was performed to remove the tumor, a resection of more than 95%. During the operation, a displacement of the neoplasm with affecting the pyramidal tract (about 8 mm) was found. On the third day after the operation, my sister was already perfectly normal, feeling quite satisfactory. At the end of May, a course of radiation therapy began, 6 weeks (TMZ 75 mg / m2 per day, concomitant radiotherapy 59-60 Gy). Immediately upon completion of the course, edema began to develop, tumor recurrence was recorded, and the condition began to deteriorate steadily. The size of the new tumor at that time was already slightly larger than the removed one. We attribute the deterioration of the condition to the consequences of therapy, since a month and a half from the operation to the start of therapy, everything was fine. As a result, the sister began to choke, it became difficult for her to walk and talk, constantly lacking oxygen. Dexamethasone 12-8 mg began to be used. In July, we had an MRI in one of the best clinics in Germany (where the first operation, radiation, chemotherapy was performed), as a result of which German doctors refused us and gave us a couple of weeks ... By the end of July, she practically stopped moving on her own, could only reach from the bed to the toilet and vice versa, her left arm was almost inactive. In August, we started using Optune, took a chemotherapy course (TMZ, 240 mg / m2 for 5 days). In early September, literally a day after the completion of chemotherapy, the condition became critical, she simply did not wake up in the morning. Doctors were able to perform a miracle, brought back to life. And they insisted on a second operation, which became, as it turned out, the last available opportunity to save her life (without an operation, it's a matter of days). The operation was carried out on September 13, the tumor was removed by 90%. Dexamethasone 3 days before surgery - 20 mg, now reduced to 5 mg. A biopsy revealed that the removed tissue is radiation necrosis. But doctors can not be sure about the remaining 10% - this is necrosis or nevertheless a tumor. After the operation, the sister successfully recovers, the doctors are satisfied with the process. Memory, speech, motor functions were not affected. Now she can take several dozen steps a day with support. Every day we work out with a fitness trainer, two days ago we started going to the pool and exercise on a stationary bike. A few days ago MRI was done, the tumor does not develop, the displacement decreased by half.
And now the main thing. We need to decide on the next steps. We wanted to participate in poliovirus trials in the USA, but they refused (complex tumor location, low Karnowski score).
Considered as options for participation in studies of the Canadian vaccine VAL-083 (interested, because its effect does not depend on MGMT methylation), the DCVax vaccine. But at the moment for us it is all inaccessible in connection with the functional state of the patient.
In addition, immediately after the second operation, we sent the tumor material for the manufacture of the dendritic vaccine. Our neurosurgeon (who performed the second operation) spoke out against its use. But we still plan to try it. Avastin was abandoned, and in general, we are actively studying alternative medicine options, we want to make our own cocktail. But while we still haven’t figured it out enough, we don’t understand how to correctly compile it, what additional information is needed for this. It’s very scary to harm her! We are afraid of the traditional treatment, because before our eyes a person literally died away with its use. And now, every day, even small, but progress and improvement is noticeable. And we are afraid to make a mistake in the independent choice of funds - what if she suddenly gets worse?
Do you believe in alternative methods in general or choose traditional treatment?
Has anyone tried soda solutions, what do you think of this method?
I understand that the question is very vague, that everything is very individual, and now I’m carefully studying all the information on the blog, but maybe you can recommend which drugs you should definitely pay attention to? What worked for many?
We will be very grateful for your reply!
Do you believe in alternative methods in general or choose traditional treatment?
Has anyone tried soda solutions, what do you think of this method?
I understand that the question is very vague, that everything is very individual, and now I’m carefully studying all the information on the blog, but maybe you can recommend which drugs you should definitely pay attention to? What worked for many?
We will be very grateful for your reply!
Monday, 14 October 2019
Feedback on Cocktail & Post-TMZ
Dear Stephen, Dear All,
I’m so sad that so many of us are finding ourselves here. You have my immense gratitude, Stephen, for the invaluable knowledge that you share with us all and for this incredible website.
I was diagnosed with GBM in July 1018. I’m a single parent of a young child. This nightmare has been devastating.
My tumor was very large, in my right parietal cortex, 100% resected. It was 94% MGMT methylated. It had TP53 mutations in three variants, no IDH1 mutation, CBL mutations in two variants, CDKN2A/CDKN2B homozygous deletions, Stag2 mutation, PDGFRA mutations in two variants (one with 85% frequency), and very high amplification of PDGFRA (~25,000 reads (>50x)) .
I’m now completing my 12th TMZ maintenance cycle. I have not yet had a recurrence and know it’s a race against the clock. The tumor sample was unfortunately set in paraffin, so I’m not a candidate for DCVax-L. I’ve been trying to raise funds for the CeGaT peptide, but coming up with all that money is a longshot for me.
1] Does anyone know if there are any other vaccines/immunotherapies for which I might qualify?
2] I’m wondering if anyone could provide a recommendation of what treatment to pursue after a year of TMZ. I battled with my neuro-onc to use CCNU on day 1 of my TMZ maintenance cycles, but she would not relent. In fact, she has refused every request I’ve made of adding agents in addition to TMZ, such as Keytruda, to prolong my survival. Is my only option at this point in terms of ‘standard of care’ metronomic low-dose TMZ?
3] Is there such a treatment as metronomic low-dose CCNU? If not, might I push to now receive CCNU in a conventional manner, assuming my blood counts are okay?
4] If I proceed with metronomic low-dose TMZ, should I avoid low-dose metronomic Accutane?
5] I had to stop high-dose Tamoxifen owing to concerning side effects. Would it have any value (such as for protein kinase inhibition) at a much lower dosage? Is there another effective anti-angiogenesis medication to use instead?
Following is my current daily combination of off-label medications. I would so greatly appreciate any feedback on the dosages (are my current ones at therapeutic levels?) and what agents I might consider adding. Thank you so very much!
Celebrex 400 mg
Metformin 1500 mg
DCA 1000 mg (on/off owing to significant neuropathy)
Lansoprazole 30 mg (120 mg 3 days before TMZ, during, 2 days after)
Chloroquine 250 mg
Naltrexone 4.5 mg
Minocycline 200 mg
Melatonin 20 mg
With gratitude and praying for us all!
~Joule
I’m so sad that so many of us are finding ourselves here. You have my immense gratitude, Stephen, for the invaluable knowledge that you share with us all and for this incredible website.
I was diagnosed with GBM in July 1018. I’m a single parent of a young child. This nightmare has been devastating.
My tumor was very large, in my right parietal cortex, 100% resected. It was 94% MGMT methylated. It had TP53 mutations in three variants, no IDH1 mutation, CBL mutations in two variants, CDKN2A/CDKN2B homozygous deletions, Stag2 mutation, PDGFRA mutations in two variants (one with 85% frequency), and very high amplification of PDGFRA (~25,000 reads (>50x)) .
I’m now completing my 12th TMZ maintenance cycle. I have not yet had a recurrence and know it’s a race against the clock. The tumor sample was unfortunately set in paraffin, so I’m not a candidate for DCVax-L. I’ve been trying to raise funds for the CeGaT peptide, but coming up with all that money is a longshot for me.
1] Does anyone know if there are any other vaccines/immunotherapies for which I might qualify?
2] I’m wondering if anyone could provide a recommendation of what treatment to pursue after a year of TMZ. I battled with my neuro-onc to use CCNU on day 1 of my TMZ maintenance cycles, but she would not relent. In fact, she has refused every request I’ve made of adding agents in addition to TMZ, such as Keytruda, to prolong my survival. Is my only option at this point in terms of ‘standard of care’ metronomic low-dose TMZ?
3] Is there such a treatment as metronomic low-dose CCNU? If not, might I push to now receive CCNU in a conventional manner, assuming my blood counts are okay?
4] If I proceed with metronomic low-dose TMZ, should I avoid low-dose metronomic Accutane?
5] I had to stop high-dose Tamoxifen owing to concerning side effects. Would it have any value (such as for protein kinase inhibition) at a much lower dosage? Is there another effective anti-angiogenesis medication to use instead?
Following is my current daily combination of off-label medications. I would so greatly appreciate any feedback on the dosages (are my current ones at therapeutic levels?) and what agents I might consider adding. Thank you so very much!
Celebrex 400 mg
Metformin 1500 mg
DCA 1000 mg (on/off owing to significant neuropathy)
Lansoprazole 30 mg (120 mg 3 days before TMZ, during, 2 days after)
Chloroquine 250 mg
Naltrexone 4.5 mg
Minocycline 200 mg
Melatonin 20 mg
With gratitude and praying for us all!
~Joule
Wednesday, 9 October 2019
Intense itching. could it be due to a supplement?
Advice and experience sought.
Having completed 6.5 weeks of radiotherapy and daily temozolomide for a grade 3 astrocytoma, I started to develop fairly intractable itching - sometimes on my legs, arms or back (which is where it is currently). It started fleetingly while I was going through the treatment, so I assumed it was a reaction to temozolomide. My blood tests were all fine when I had my last dose of treatment. It's been over two weeks since my last dose of temozolomide and the itching is getting worse. I wondered whether anyone had experienced such symptoms with any of the following cocktail?
Having completed 6.5 weeks of radiotherapy and daily temozolomide for a grade 3 astrocytoma, I started to develop fairly intractable itching - sometimes on my legs, arms or back (which is where it is currently). It started fleetingly while I was going through the treatment, so I assumed it was a reaction to temozolomide. My blood tests were all fine when I had my last dose of treatment. It's been over two weeks since my last dose of temozolomide and the itching is getting worse. I wondered whether anyone had experienced such symptoms with any of the following cocktail?
- Boswellia (WokVel): 999mg / day
- Vitamin D: 10,000IU / day
- Curcumin (Longvida): 1000mg/day
- ECGC (TeaVigo) Green tea extract 1/day
- Melatonin: 20mg at night
- Omega 3 Fish Oils: 3000mg daily of EPA +DHA
- Chloroquine phosphate 250mg/ day
- Selenium: 200mcg/day
- Etodolac: 600mg/day
- CBD oil: 50mg+ / day
I'm going to see my family doctor to check whether it is anything obvious, and to get kidney and liver function blood tests done.
Any other ideas or suggestions?
Monday, 7 October 2019
URGENT: my son of 6. Help needed with decision and protocol
Dear friends,
I have a very delicate and urgent decision to make tomorrow and i would love to hear what you think. I think nobody can understand us better than you.
My son of 6, Dario, is diagnosed with an aggressive brain tumor called AT/RT in the 4th posterior fossa. At the time od diagnosis he had a M1 metastasis consiting of cells found in the spine. After this diagnosis all the spine test were negative (done every month). He had surgery in may 2018 and we followed the sickkids protcol for a year and a few months (6 cycles of chemotherapy and maintenance protocol consisting of tamoxifen)
After 1.3 years he relapsed this last 29 august and he had again surgery with total resection. The tumor came back in the same.
After the relapsed i started to devour all the literature and find these non conventional approaches and researches like Daniel from cancertreatmentresearch.com who are helping us.
We started a off label drugs cocktail that i have pasted bellow. We are following this religiously. And we are triying to improve it. A pediatric doctor and some other researches are helping us to find dosages etc
The MRI two weeks ago is clean and the CT scan from thursday is clean but since we have not done any chemo or radio after surgery, we are nervous.
Our oncologist at the hospital only recommend at this point doing full brain and spine proton irradiation (54gy in the tumor bed) and 34gy in the spine and rest of the brain.
For a kid of 6 year this is not the best treatment but it is also an aggresive cancer. So most of the standard oncologist and radiologist will recommend this standard treatment. We never did radiation before.
So, my line of thinking is untill now:Let's do focal radiation only and give him the opportunity to avoid serious side effects of the full brain and spine irradjatiob and if the tumor comes back, we are using the off-label drugs and a second irradiation only to where the tumor if it comes.
I am still in doubt, my wife too. I do not know i we are risking his life or not. If we do not irradiate the whole brain, there is the risk of dissemination because he already had M1 at diagnosis and after one month he has not received any chemo or radiation.
I don't want to make you responsible of giving your opinion because we are the ones responsible but i am not sure if the tumor come backs we can fight it with the "off-label drugs". Since it is aggressive and comes very fast, i do not have experience what you could have had in brain tumors or your collegues in this world of non-conventional treatments. There is also metronomic treatments or alisertib for re-ocurrences.
Please, help me. I will never make you responsible of any suggestion but you have seen many cases already of this type, can you comment what is your view? what will you if it was your son?
I am trying to give him an opportunity to avoid the big side effects of total radiotherapy but at the same time i am not sure if we are risking his life.
We have time and resources to dedicate for him.
This is what we are following now:
===
PROTOCOL
Thanks in advance
I am trying to give him an opportunity to avoid the big side effects of total radiotherapy but at the same time i am not sure if we are risking his life.
We have time and resources to dedicate for him.
This is what we are following now:
===
PROTOCOL
Main drugs used now:
- METFORMIN 500mg 1/2 pill after breakfast daily for 2 weeks if tolerated increase to 1 pill after breakfast daily
- MEBENDAZOLE 200mg 1 pill after lunch daily
3. ATORVASTATIN or sinvastim 10mg 1 pill at bedtime
4. DOXYCYCLINE 100mg 1 pill after dinner for 30 Days EVERY 3 MONTHS, to start after 3 MONTHS.
5. TAGAMET (CIMETIDINE) 200mg 1 pill once daily {PLEASE DO NOT TAKE WITH ANY OTHER MEDICATIONS, VITAMINS, OR SUPPLEMENTS}
6. CLARITIN (LORATADINE) 10mg 1 pill once daily
7. NICLOSAMIDE 500mg 1 pill once daily THREE TIMES WEEK ONLY (we have not started this drug)
8. IBUPROFEN 200mg 2x/day after food (PULSE THERAPY which means doing this periodically for 2-3 months at a time with breaks of 1-2 months. We have not started this one)
9, Oral etoposide (we started this one 2 days back)
9, Oral etoposide (we started this one 2 days back)
Drugs that will being considered depending on outcomes and safety of use:
- Ribavirine. 200 mg.
- Disulfiram modulates stemness and metabolism of brain tumor initiating cells in atypical teratoid/rhabdoid tumors https://academic.oup.com/neuro-oncology/article/17/6/810/1113353
- 6-diazo-5-oxo-L-norleucine. Unbiased metabolic profiling predicts sensitivity of high MYC-expressing atypical teratoid/rhabdoid tumors to glutamine inhibition with 6-diazo-5-oxo-L-norleucine https://clincancerres.aacrjournals.org/content/early/2019/07/12/1078-0432.CCR-19-0189
- Dasatinib and nilotinib
differential methylation of a PDGFRB-associated enhancer confers specific sensitivity of group 2 ATRT cells to dasatinib and nilotinib, and suggest that these are promising therapies for this highly lethal ATRT subtype. https://www.cell.com/cancer-cell/pdf/S1535-6108(16)30509-8.pdf https://www.ncbi.nlm.nih.gov/pubmed/27960086 - Sustained Complete Response to Metronomic Chemotherapy in a Child with Refractory Atypical Teratoid Rhabdoid Tumor: A Case Report https://www.frontiersin.org/articles/10.3389/fphar.2017.00792/full
Continuous oral celecoxib with alternating metronomic etoposide and cyclophosphamide, in combination with biweekly bevacizumab and monthly intrathecal liposomal cytarabine - Inositol tripuorosphosphate. Method of reducing multi-drug resistance
7, Phenylbutyrate to Treat Children With Progressive or Recurrent Brain Tumors https://clinicaltrials.gov/ct2/show/NCT00006450.
9, valganciclovir A Swedish study used a loading dose, followed by a maintenance dose. The loading dose was 900 mg orally twice a day for three weeks, followed by 900 mg a day. Valcyte tablets come in 450 mg tablets so that would be 2 tablets in the morning and in the evening for 3 weeks and then 2 tablets in the morning thereafter every day
10.chloroquine/mefloquin
10.chloroquine/mefloquin
11. clemastine
SUPPLEMENTS used now
8. CURCUMIN 400mg 1 pill 2x/day
9. BOSWELLIA 400mg must be a minimum of 3000mg per day (8 pills per day)
10. VITAMIN D 3000 IU once daily
11. PROBIOTIC once daily
12. ASHWAGHANDA 500mg 1 pill 2x/day
13. MUSHROOM EXTRACT 2x/day
14. MILK THISTLE 175mg 1pill once daily
15. ASTRAGALUS 500mg 1 pill 2x/day [During Radiation Increase to 2 pills 3x/day]
16. URSOLIC ACID 50mg once daily hay 150
17. CBD-THC. 1:1 ratio.
Supplements that are being considered:
a) Magnesium gluconate supplement https://www.cancertreatmentsresearch.com/an-anti-cancer-compound-hiding-in-front-of-us-gluconate/
b) Silver solution https://www.cancertreatmentsresearch.com/a-silver-bullet-to-kill-cancer/
c) Canagliflozin https://www.cancertreatmentsresearch.com/glucose-absorption-inhibitors-to-inhibit-tumor-growth/ The purpose of using this one is to lower the amount of glucose absorbed by the tumor
D) Honokiol. Eliminates Glioma/Glioblastoma Stem Cell-Like Cells Via JAK-STAT3 Signaling and Inhibits Tumor Progression by Targeting Epidermal Growth Fac..https://www.ncbi.nlm.nih.gov/pubmed/30587839/
d) Fish oil. 1000 mg (w/ any meal, unless PLT < 125)
E) Artemisia annua
f) Melatonine, 5b (built gradually)
g) Digestive enzymes (with each meal)
H) Essiac (night)
i) Selenium, 50-75mcg
Thanks in advance
Óscar
Thursday, 26 September 2019
Repurposing perampanel (glutamate receptor blocker)?
About a week ago there was a major study published in the journal Nature called "Glutamatergic synaptic input to glioma cells drives brain tumour progression".
https://www.ncbi.nlm.nih.gov/pubmed/31534219
I've uploaded the full study to the Pathology folder in the Brain Tumor Library.
The study discovers a communication network between neurons and glioma cells, with certain effects (including tumor invasiveness) mediated by AMPA type glutamate receptors. Furthermore, these effects were blocked in vitro by the approved AMPA glutamate receptor antagonists, perampanel.
Perampanel was approved in 2012 for partial seizures and generalized tonic-clonic seizures for people older than 12 years, so could also have anti-seizure effects in addition to potential anti-tumor effects.
The relevant discussion from the Nature paper is as follows:
The selective non-competitive AMPAR antagonist perampanel is an approved antiepileptic drug shown to have potential antitumour effects in patients with glioma and warrants further investigation. Chronic administration of perampanel to xenografted mice decreased the proliferation of GB cells as determined by in vivo imaging of tumour regions over time (Fig. 5j, k, Extended Data Fig. 9a) independently of cell-autonomous effects as determined by an in vitro proliferation assay (Extended Data Fig. 9b).
This is not the first paper to discuss perampanel effects on glioma and/or seizure control for glioma patients. For example:
AMPA receptor antagonist perampanel affects glioblastoma cell growth and glutamate release in vitro
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0211644
Adjunctive perampanel for glioma-associated epilepsy.
https://www.ncbi.nlm.nih.gov/pubmed/30377587
https://www.ncbi.nlm.nih.gov/pubmed/31534219
I've uploaded the full study to the Pathology folder in the Brain Tumor Library.
The study discovers a communication network between neurons and glioma cells, with certain effects (including tumor invasiveness) mediated by AMPA type glutamate receptors. Furthermore, these effects were blocked in vitro by the approved AMPA glutamate receptor antagonists, perampanel.
Perampanel was approved in 2012 for partial seizures and generalized tonic-clonic seizures for people older than 12 years, so could also have anti-seizure effects in addition to potential anti-tumor effects.
The relevant discussion from the Nature paper is as follows:
The selective non-competitive AMPAR antagonist perampanel is an approved antiepileptic drug shown to have potential antitumour effects in patients with glioma and warrants further investigation. Chronic administration of perampanel to xenografted mice decreased the proliferation of GB cells as determined by in vivo imaging of tumour regions over time (Fig. 5j, k, Extended Data Fig. 9a) independently of cell-autonomous effects as determined by an in vitro proliferation assay (Extended Data Fig. 9b).
This is not the first paper to discuss perampanel effects on glioma and/or seizure control for glioma patients. For example:
AMPA receptor antagonist perampanel affects glioblastoma cell growth and glutamate release in vitro
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0211644
Adjunctive perampanel for glioma-associated epilepsy.
https://www.ncbi.nlm.nih.gov/pubmed/30377587
Feasibility of modified Atkins diet during radiation - retrospective study
Feasibility of a modified Atkins diet in glioma patients during radiation and its effect on radiation sensitization.
https://www.ncbi.nlm.nih.gov/pubmed/31548811
https://www.ncbi.nlm.nih.gov/pubmed/31548811
Monday, 23 September 2019
Avastin alone?
Further to a recent previous post.
3 months of TMZ 5/23 showed that chemo is not working for unmethylated GBM. The tumor is very active according to MRI comparison between July and September 2019. There was alot of swelling which is currently being reduced with 16 mg steroids per day in the past week. Speech has improved alot with this. Was told it is too close to previous radiation or surgery to have either done again.
2 weeks ago clonazepam was prescribed 10mg x 2 and Keppra increased to 1500mg x 2 and Phenytoin 300mg in the morning - all of this is keeping seizures, twitches and focal seizures away.
Oncologist is going to start IV Avastin today and stop all treatment - asked if it was pallatiative but answer no it is not pallatiative treatment yet. Thought it was unusual to go ahead with Avastin by itself and not combine it with another chemo treatment such as lomustine?
Have been following cocktail since during radiation treatment back in April 2019 which I posted about in previous post. This includes daily chloroquine (155mg active ingredient); celebrex 200mg; metformin 500mg x 2; Atorvastatin; ramipril; ranitidine 75 mg; mebendazole; melatonin 20mg.
Also the usual daily supplements of mulitvitamin; 16 strain Probiotics; PSK; Maitake D; ; Mushroom supplement mix for brain (lions mane 300mg; bacopa 250 mg; reishi 150 mg; gotu kola 130 mg; ginko 120 mg); curcumin (longvida); vitamin D; ECG; Milk Thistle; Berberine; Boswellia; Resveratrol; Omega 3-6-9; Soy Falvonoids (geinistein)
Wondering if anyone has any experience of just Avastin being prescribed? I am wondering what is even the point in doing avastin alone? Appears to have more side effects and very little extra benefits, or OS? I was optimistic that Richard Geiber had Avastin and low dose TMZ but that doesnt seem to be on offer to us? Or any chemo alternative?
Very disappointing TMZ stupps protocol + cocktail did not seem to work.
3 months of TMZ 5/23 showed that chemo is not working for unmethylated GBM. The tumor is very active according to MRI comparison between July and September 2019. There was alot of swelling which is currently being reduced with 16 mg steroids per day in the past week. Speech has improved alot with this. Was told it is too close to previous radiation or surgery to have either done again.
2 weeks ago clonazepam was prescribed 10mg x 2 and Keppra increased to 1500mg x 2 and Phenytoin 300mg in the morning - all of this is keeping seizures, twitches and focal seizures away.
Oncologist is going to start IV Avastin today and stop all treatment - asked if it was pallatiative but answer no it is not pallatiative treatment yet. Thought it was unusual to go ahead with Avastin by itself and not combine it with another chemo treatment such as lomustine?
Have been following cocktail since during radiation treatment back in April 2019 which I posted about in previous post. This includes daily chloroquine (155mg active ingredient); celebrex 200mg; metformin 500mg x 2; Atorvastatin; ramipril; ranitidine 75 mg; mebendazole; melatonin 20mg.
Also the usual daily supplements of mulitvitamin; 16 strain Probiotics; PSK; Maitake D; ; Mushroom supplement mix for brain (lions mane 300mg; bacopa 250 mg; reishi 150 mg; gotu kola 130 mg; ginko 120 mg); curcumin (longvida); vitamin D; ECG; Milk Thistle; Berberine; Boswellia; Resveratrol; Omega 3-6-9; Soy Falvonoids (geinistein)
Wondering if anyone has any experience of just Avastin being prescribed? I am wondering what is even the point in doing avastin alone? Appears to have more side effects and very little extra benefits, or OS? I was optimistic that Richard Geiber had Avastin and low dose TMZ but that doesnt seem to be on offer to us? Or any chemo alternative?
Very disappointing TMZ stupps protocol + cocktail did not seem to work.
Friday, 6 September 2019
CUSP9v3. Gliovac. Toca 511
Dear Stephen, dear all!
1) What do you think about GLIOVAC(https://www.erc-immunotherapy.com/products/gliovac-erc1671)?
And about DCVax?
What is the difference between them?
And there is also dendritic cell vaccine in IOZK (the cheapest one).
Which one has better statistics? Is it worse trying?
1) What do you think about GLIOVAC(https://www.erc-immunotherapy.com/products/gliovac-erc1671)?
And about DCVax?
What is the difference between them?
And there is also dendritic cell vaccine in IOZK (the cheapest one).
Which one has better statistics? Is it worse trying?
2) What about CUSP9v3 protocol effectiveness? Want to try it for my mom. A lot of discussions here in the blog, but can't find information about latest clinical trials results.
3) What do you think about Toca 511? Any experience?
Thank you!
Cocktail question, Fluoxetine or Celebrex?
Dear Stephen and all,
I have a question concerning my girlfriend's father. He is 57 years old. He was diagnosed with a Grade IV, MGMT unmethylated Glioblastoma in the left occipital lobe, September 2018. After the surgery, he received radiotherapy and chemotherapy using VAL-083 in China during 08/11/2018 - 27/06/2019. He had an MRI scan on 20/08/2019 and there is a 17mm*10mm GBM recurrence in the left temporal lobe.
Now his oncologist suggests receiving the standard 5/23 Temozolomide treatment. Since his GBM is MGMT unmethylated, we want to have the cocktail to enhance the performance of Temozolomide for him. He is taking Metformin, Verapamil, Chloroquine and Keppra. We want to choose 1 more medicine from Fluoxetine and Celebrex, which one is better?
Thank you for your help! Best wishes to everyone.
Details of the condition of my father are listed below:
I have a question concerning my girlfriend's father. He is 57 years old. He was diagnosed with a Grade IV, MGMT unmethylated Glioblastoma in the left occipital lobe, September 2018. After the surgery, he received radiotherapy and chemotherapy using VAL-083 in China during 08/11/2018 - 27/06/2019. He had an MRI scan on 20/08/2019 and there is a 17mm*10mm GBM recurrence in the left temporal lobe.
Now his oncologist suggests receiving the standard 5/23 Temozolomide treatment. Since his GBM is MGMT unmethylated, we want to have the cocktail to enhance the performance of Temozolomide for him. He is taking Metformin, Verapamil, Chloroquine and Keppra. We want to choose 1 more medicine from Fluoxetine and Celebrex, which one is better?
Thank you for your help! Best wishes to everyone.
Details of the condition of my father are listed below:
- On 28/09/2018 he had surgery due to a tumor in the left occipital lobe. According to the biopsy, he was diagnosed with a Grade IV Glioblastoma Multiforme, MGMT unmethylated, ki67 70%, IDH1/2(-), 1p/19q non-codeleted, non-diffuse.
- On 08/11/2018, he began to receive radiotherapy and chemotherapy using VAL-083 with a dose of 30mg/m2 IV. But soon he suffered severe myelosuppression and both radiotherapy and chemotherapy are stopped for 2 weeks. After that, the dose of VAL-083 was tuned to 20mg/m2.
- On 24/06/2019, the assessment via MRI is CR I class, complete response (that shows the VAL-083 is effective for him)
- On 27/06/2019, he finished the clinical trial, including 10 cycles of treatment using VAL-083.
- On 20/08/2019, MRI shows that there is a 17mm*10mm enhanced mass in the left temporal lobe (the original tumor was in left occipital lobe).
Monday, 19 August 2019
Urgent help for an 11 year old girl
Dear
Stephen and all,
I have a
question concerning my friend’s daughter. She is a Spanish 11 year old girl.
She has been diagnosed with a grade IV medular glioma. She had surgery, but the
tumor could not be removed. They just took a biopsy. She has had 30 sessions of
radiation and 27 days of temozolomide. Parents are desperatly looking for
possible clinical trials that would fit her case. Any suggestions on specific
treatments or cocktails would be of much help as well. Even though they live in
Spain they would have no problem travelling overseas. We are attaching
pathological report, MRI and tractography report.
Please click on the following link. Once the link takes you to the page of the girl's medical information, click on "Visualizar el estudio" to see her images and "Descargar el informe" to read the medical report:
http://resultados.healthtime.es/PortalPaciente/OpenSharedStudyRequest/a4ac550a-19f7-4d58-99ad-6e1fb2e06ccb
The picture I am including is the report of the pathologist. It is in Spanish, but I think it is understandable. If you have any questions, please contact me.
Thank you all in advance.
Isabel
Cocktail questions, also foot twitching?
My dad aged 59 had a grand mal seizure 25th Feb 2019; operation/debulking 7th March 2019, Radiochemotherapy 30 sessions in May 2019. Completed 2nd round of 5/23 chemo cycle. He is negative for IDH, MGMT.
Overall he has been doing ok with the treatment. The only set back was when he had around 3 to 4 multiple grand mal seizures around 30th June 2019. We had no warning about that seizure and our medical team didn't warn us that he could get seizures from the radiation swelling 4 weeks post radiation (we thought maybe just during radiation treatment). He had no side effects during radiation treatment period itself - we were shocked that it happened -
Question 1: Seizures post radiation 4 weeks after radiation
I guess it is a "normal" side effect? We thought seizures would be a side effect later on when the treatment might stop working. The hospital put him into an induce coma for 2 days to stop the seizures. He took steroids for about 6 weeks after and has come off the steroids now and has had no further seizures. We are also surprised that nobody ever mentioned to us to have buccal midazolam injection at hand as when we called the ambulance, the paramedics had to call the fire brigade for an advance paramedic to inject IV anti seizure drug. If we had the buccal midazolam this might have prevented the multiple seizures. He now carries the buccal midazolam injections around.
Question 2: Foot twitching post seizure, same side as tumor
His Keppra was 2 x 500mg up until then and now they have increased it to 2.5g per day and added Phenytoin. Since that seizure he has had a foot twitch during the night and a sore pain in his thumb - can be normal effects from the swelling and tumor? The tumor is on the left side and the twitch is on the left side which is unusual? The doctors would expect the tumor to effect the right side.
We stopped doing the cocktail after 30th June with the big seizure then but then continued with Chloroquine and Celebrex a week later. We have since started back doing the cocktail (see below).
Question 3: Celebrex
I read the Brain Tumor Charity do not support taking Celebrex and some articles says it is not good to take, what is the opinion about it now given the new clinical trail data? Also it seems like it can react with Epainutin (Phenytoin) so we give it to him in the evening. - https://www.thebraintumourcharity.org/brain-tumour-diagnosis-treatment/treating-brain-tumours/treatments-licensed-other-illnesses/celecoxib-celebrex/
Question 4: Daily timetable of cocktail
Do people have a daily timetable to avoid interactions between anti-seizure drugs and others?
Question 5: Disulfiram
We have disulfiram but we have never given it to him as it seems to interact with the Epanutin (Phenytoin). Have people taken this together?
Question 6: Curcumin
He is taking Doctors Best High absorption Curcumin with C3 Complex and Bioperin 1000 mg. This tablet he finds hard to digest because it is very big and solid even using a tablet cutter. Is there a different brand which people recommend which is easier to take?
Question 7: Reishi
He is taking Reishi as part of a multi-mushroom supplement for Brain function called Fungi Perfecti, MycoBotanicals for the Brain. However we read on Sloan Kettering that reishi is not good to take?
Question 8: Ranitidine in absence Cimetidine
He is taking Ranitidine as we could not get cimetidine. We asked a friend in Spain to get the cimetidine but they got us cinitaprida normon? It is for treating stomach ulcers but I guess its totally different as it doesn't appear to be a H2 antihistamine. We were not sure if it was any use giving it to my dad? We have not given him the Cinitaprida normon but we give him 75mg Ranitidine a day.
Question 9: Mebendazole
He is taking Mebendazole 100mg daily - i know its well below the dosages a human would need to take compared to the mouse study? Do people take much higher doses? The studies do not seem clear about it but I know it is used in Care Oncology alot?
Question 10: Antibiotics Doxycycline/Minocycline
Antibiotics – he was only on these when during radiochemo phase but not now…Care oncology seems to recommend doxycycline and a rotation with other antibiotics such as minocycline? Should he start taking this too? How much do people take, do people rotate each month? Surely antibiotics will cancel out the effects of building up the immune system?
Question 11: Valacyclovir and other antiviral drugs?
Should we look into taking Valacyclovir? (I know there is no right or wrong cocktail). If so, how do people get this, how long do they take it for? We read somewhere that people can get tested for different virus's in their system such as Herpes? Is there a test for CMV? Is there any other herpes/CMV drugs we should take?
Question 12: Amino acid Brain supplements L-tyrosine and N-acetyl cysteine
We had been giving him L-tyrosine and N-acetyl cysteine and we stopped after the seizure. I know Cheryl Broyle mentioned using NAC. I don't know if these 2 compounds have good/bad effects on the brain? For a normal brain they are meant to be good.
Question 13: Vitamin C IV
I read up on Vitamin C IV and I don't know if we should try that - it doesn't seem clear if it is effective or not and it doesn't mention it could flush out the anti-seizure drugs?? Those studies mention N-acetyl cysteine reverses the benefits of IV Vit C??
Question 14: Berberine
Only recently ive seen many people taking berberine. Are many people taking this supplement?
Question 15: Other Repurpose drugs
Interesting article with a few extra repurpose drugs which I have not mentioned above. Not too familar with them and the cocktail?
Prescribed by GB:
Keppra - Anti seizure. he was on 500 mg x 2 day but since the seizure it is now 2.5g per day.
Keppra - Anti seizure. he was on 500 mg x 2 day but since the seizure it is now 2.5g per day.
Epanutin - Phenytoin. Anti seizure..100 mg x 3
Atorvastatin – Cholesterol treatment 20 mg per day
Metformin – diabetic, 500 mg twice a day
Ramipril - To lower blood pressure, 5mg
Atorvastatin – Cholesterol treatment 20 mg per day
Metformin – diabetic, 500 mg twice a day
Ramipril - To lower blood pressure, 5mg
Melatonin 20 mg
Off-label prescription/non prescription drugs:
- Chloroquine Phosphate, 250 mg/day
- Celebrex (Celecoxib), 200 mg/day
- Mebendazole 100mg - this is the recommended daily dose for normal pinworm treatment but i read people are on more?
- We could not get Tagamet (cimetidine), so we were using Ranitidine, another Histamine H2 receptor (usually used for stomach uclers - repurpose of Cimetidine is immune, anti invasion. We do not know if Ranitidine is a good replacement but apparently cimetidine can interact with Celebrex, but I think Ranitidine has reduce side effects to Tagamet). - we have not restarted Ranitidine yet
Supplements: Majority of these we get from iherb apart from the coriolus versicolor which we order from evitamins.
- Coriolus versicolor extract PSK/PSP (Turkey tail mushroom)
- Maitake-D mushroom extract, 1200mg per day
- Reishi mushroom extract - for immune. We got Fungi Perfecti mycobotanicals for the Brain
- Curcumin High absorption extract 1000mg
- Omega-3-6-9 1200 mg
- Boswellia extract 500 mg – to reduce edema
- Standard multivitamin/multimineral capsules, time-release
- Probiotic (Garden of Life, Dr. Formulated Mood+ 16 strains)
- Vitamin D, 5,000 IU/day
- Selenium (we just used a multi purpose vitamin)
- Soy Extract (we were using Soya Isoflavonoids which I think contains genistein which is meant to be good).
- Resveratrol 200mg
- Green Tea Extract ECGg 400 mg
Supplements: Majority of these we get from iherb apart from the coriolus versicolor which we order from evitamins.
- Coriolus versicolor extract PSK/PSP (Turkey tail mushroom)
- Maitake-D mushroom extract, 1200mg per day
- Reishi mushroom extract - for immune. We got Fungi Perfecti mycobotanicals for the Brain
- Curcumin High absorption extract 1000mg
- Omega-3-6-9 1200 mg
- Boswellia extract 500 mg – to reduce edema
- Standard multivitamin/multimineral capsules, time-release
- Probiotic (Garden of Life, Dr. Formulated Mood+ 16 strains)
- Vitamin D, 5,000 IU/day
- Selenium (we just used a multi purpose vitamin)
- Soy Extract (we were using Soya Isoflavonoids which I think contains genistein which is meant to be good).
- Resveratrol 200mg
- Green Tea Extract ECGg 400 mg
- Silymarin
Stopped taking - should we take again?
- NAC N-acetyl cysteine– I noticed Cheryl Broyle was taking this but it is not on Stephen’s cocktail list.
- L-Tyrosine 500mg – I did not see this on any cocktail list but it is an amino acid which is meant to help with brain function.
- L-Tyrosine 500mg – I did not see this on any cocktail list but it is an amino acid which is meant to help with brain function.
Never started this but should we after the seizure? Can it interfere?:
- Disulfiram and he has not started this.
Low Level Dex Long-Term/Indefinitely
Hello,
I'm hoping to interact with those who have needed to stay on Dex long-term at low levels (2mgs or less) or hear from experts on the topic.
My Uncle was on very high levels for many months but we've not gotten him down to 2mgs and it seems that going lower is not an option to do - safely. He had regrowth immediately after surgery, that said he's got tumors in his head taking up space, and also at this point his adrenals are shot.
I imagine that just like any drugs the lower the level, the less detrimental they are.
Is anyone on 2mgs or less - indefinitely?
Thanks :)
I'm hoping to interact with those who have needed to stay on Dex long-term at low levels (2mgs or less) or hear from experts on the topic.
My Uncle was on very high levels for many months but we've not gotten him down to 2mgs and it seems that going lower is not an option to do - safely. He had regrowth immediately after surgery, that said he's got tumors in his head taking up space, and also at this point his adrenals are shot.
I imagine that just like any drugs the lower the level, the less detrimental they are.
Is anyone on 2mgs or less - indefinitely?
Thanks :)
Wednesday, 14 August 2019
Demention. Hbot. Glioblastoma. Radiation therapy consequences.
Dear Stephen! Dear all!
My mom has demention because of hydrocephalus, as well as, probably, in connection with radiation therapy. Today she will have a shunt. However, we need to treat the consequences. One person said that in England in this case they use hbot.
My mom has demention because of hydrocephalus, as well as, probably, in connection with radiation therapy. Today she will have a shunt. However, we need to treat the consequences. One person said that in England in this case they use hbot.
Questions:
1) can hbot cause glioblastoma progression? I read that this procedure improves blood supply, because the tumor is usually well supplied with blood vessels and blood supply could it make worse? Or is it incoherent things? We are currently taking Avastin.
2) could hbot really help with demention? Any experience?
3) could you please advise other good methods to treat demention and consequences of radiation therapy? Cbd oil, lions mane, ps100?
1) can hbot cause glioblastoma progression? I read that this procedure improves blood supply, because the tumor is usually well supplied with blood vessels and blood supply could it make worse? Or is it incoherent things? We are currently taking Avastin.
2) could hbot really help with demention? Any experience?
3) could you please advise other good methods to treat demention and consequences of radiation therapy? Cbd oil, lions mane, ps100?
Thank you!
Monday, 29 July 2019
Could AstraZeneca’s ovarian cancer drug also treat glioblastoma?
This is a year and half old but I thought I'd throw it out there for the group -
https://www.fiercebiotech.com/research/could-astrazeneca-s-ovarian-cancer-drug-also-treat-glioblastoma
https://www.fiercebiotech.com/research/could-astrazeneca-s-ovarian-cancer-drug-also-treat-glioblastoma
Wednesday, 24 July 2019
A KETOGENIC PILL FOR GLIOBLASTOMA ?
Came across this study and would love to know others' thoughts. I have been following the progress of the ketogenic (almost no carbohydrate) diet for some time and its potential value in glioblastoma and epilepsy. This study seems to show that some of the purported benefits could be achieved through a ketone ester supplement, which serves to provide the brain with its alternative non-glucose fuel source (Ketone bodies)
direct link to abstract: https://academic.oup.com/neuro-oncology/article-abstract/20/suppl_6/vi36/5154383?redirectedFrom=fulltext )
Any thoughts on this, and how it might be translated to human use?
Thanks!
direct link to abstract: https://academic.oup.com/neuro-oncology/article-abstract/20/suppl_6/vi36/5154383?redirectedFrom=fulltext )
Any thoughts on this, and how it might be translated to human use?
Thanks!
Alternative to Bosellia Wokvel?
I've seen previous posts explaining the rationale behind the recommendation of Boswellia (WokVel) preparation. However, this formulation is currently out of stock from all suppliers in my area (UK). I note from Ben Williams' book that the dose of boswellia used in the cited German trial (showing reduced oedema) was 4200 mg/day, which is much higher than the 999mg suggested on this site. What's the best alternative to WokVel, given that I am unable to source it? I assume that taking it alongside Celecoxib is tried-and-tested?
Monday, 22 July 2019
Do statins, ACE inhibitors or sartans improve outcome in primary glioblastoma?
Hello all,
I spotted this paper and thought it was best to share: “Do statins, ACE inhibitors or sartans improve outcome in primary glioblastoma?” Although I’ve not read the full paper, it’s worth noting that they concluded:
I spotted this paper and thought it was best to share: “Do statins, ACE inhibitors or sartans improve outcome in primary glioblastoma?” Although I’ve not read the full paper, it’s worth noting that they concluded:
This secondary analysis of two large glioblastoma trials thus was unable to detect evidence for an association of the use of statins, ACEI or sartans with outcome in patients with newly diagnosed glioblastomaShould we abandon ACE inhibitors, etc?
Seeing feedback on proposed treatment plan and drug/ supplement cocktail
Hi Stephen,
I finally have medical data back for my dad and we had our first meeting with his oncology teams yesterday. I have summarized his medical data as well as our treatment plan below.
A couple of notes and questions upfront:
-
I didn't see anything on my dad's medical records about MGMT
-
Would greatly appreciate your feedback on the proposed drug cocktail and supplements
-
Are we missing anything?/ Dosages?
-
I would like to supplement COC protocol with some additional re-purposed drugs (particularly the first 4 in the table below. Do you have any information on dosage and how others go about getting prescriptions for these?
-
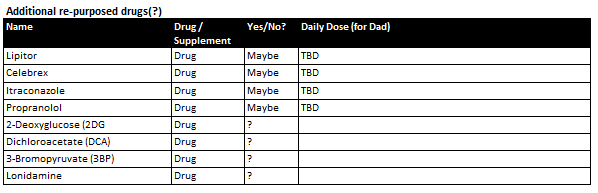
Many thanks again for your continued help.
Silvia
MEDICAL DATA:
-
Clinical synopsis
-
64M p/w expressive dyphasia and headache with likely malignant transformation of L) temporal LGG
-
2018 June generalised seizure diagnosed with left temporal mass likely LGG
-
Monitored as outpatient
-
Started on keppra and phenytoin for seizure control (self ceased keppra in
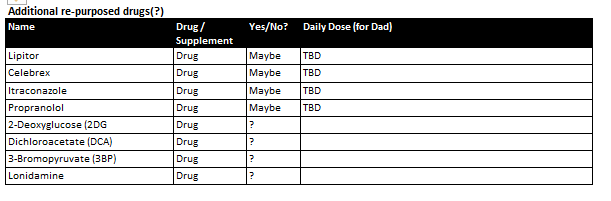 January due to rash)
January due to rash)
-
Last seizure in April
-
July 2019 clinical synopsis
-
Presented with headaches and expressive dyphasia
-
Treatment
-
Stereotactic left temporal craniotomy and debulking of glioma (3 July)
-
Good postoperative course
-
Discharged 11 July
-
Medications
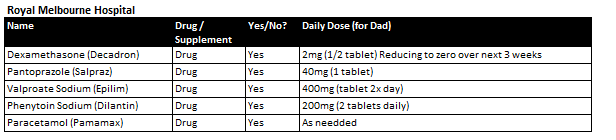
-
Histopathology results
-
Final Diagnosis: Left insula lesion: Glioblastoma. Features in keeping with IDH wild type (WHO grade IV)
-
GFAP positive
-
IDH-1 R132H negative (not mutated)
-
ATRX positive (not mutated)
-
P53 positive
-
P16 CDKN2A negative
-
Topoisomerase - approximately 20%
-
Post operative MRI
-
Small focus of residual enhancing tumour at the posterosuperior resection margin. Extensive oedema with midline shift measuring 9mm to the right and left uncal herniation has slightly improved
-
Recommending SOC treatment
-
Radiation / chemo to begin in ~3 weeks (~12 August)
-
Combined radiation & TMZ
-
Confirming targeted cavity and margin, not whole brain
-
Starting with 3 week course as patient is over 60
-
If patient is fit will recommend more aggressive 6 week treatment (TBD)
-
Followed by TMZ maintenance schedule
OUR CURRENT PLAN
-
Commence SOC protocol as prescribed by medical team in ~3 weeks
-
Complement with
-
(1) Ketogenic Diet
-
Strict 4:1 ratio, targeting Glucose / Ketone Index of 1:2 or lower (ideally 1:1 at 3mmol/ L each)
-
Calorie restricted ~900kcal/ day
-
Intermittent fasting (work towards target 2 - 8pm eating window)
-
Supplemented with Exogenous ketones (Caprilic acid and BHB salts during fasting window and can also be consumed during eating window)
-
(2) Repurposed drugs cocktail per Care Oncology Clinic (submitted info, waiting for treatment plan)
-

-
(3) Supplements
-
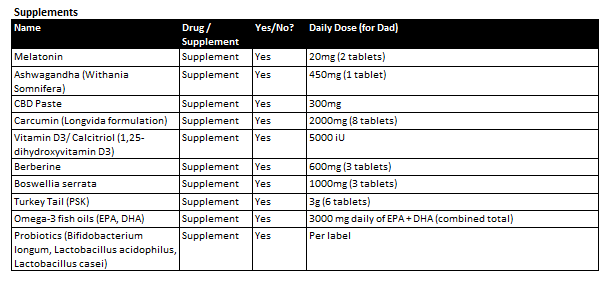
I didn't see anything on my dad's medical records about MGMT
Would greatly appreciate your feedback on the proposed drug cocktail and supplements
- Are we missing anything?/ Dosages?
- I would like to supplement COC protocol with some additional re-purposed drugs (particularly the first 4 in the table below. Do you have any information on dosage and how others go about getting prescriptions for these?
Clinical synopsis
- 64M p/w expressive dyphasia and headache with likely malignant transformation of L) temporal LGG
- 2018 June generalised seizure diagnosed with left temporal mass likely LGG
- Monitored as outpatient
- Started on keppra and phenytoin for seizure control (self ceased keppra in
January due to rash)
- Last seizure in April
- July 2019 clinical synopsis
- Presented with headaches and expressive dyphasia
- Treatment
- Stereotactic left temporal craniotomy and debulking of glioma (3 July)
- Good postoperative course
- Discharged 11 July
- Medications
Histopathology results
- Final Diagnosis: Left insula lesion: Glioblastoma. Features in keeping with IDH wild type (WHO grade IV)
- GFAP positive
- IDH-1 R132H negative (not mutated)
- ATRX positive (not mutated)
- P53 positive
- P16 CDKN2A negative
- Topoisomerase - approximately 20%
Post operative MRI
- Small focus of residual enhancing tumour at the posterosuperior resection margin. Extensive oedema with midline shift measuring 9mm to the right and left uncal herniation has slightly improved
Recommending SOC treatment
- Radiation / chemo to begin in ~3 weeks (~12 August)
- Combined radiation & TMZ
- Confirming targeted cavity and margin, not whole brain
- Starting with 3 week course as patient is over 60
- If patient is fit will recommend more aggressive 6 week treatment (TBD)
- Followed by TMZ maintenance schedule
Commence SOC protocol as prescribed by medical team in ~3 weeks
Complement with
- (1) Ketogenic Diet
- Strict 4:1 ratio, targeting Glucose / Ketone Index of 1:2 or lower (ideally 1:1 at 3mmol/ L each)
- Calorie restricted ~900kcal/ day
- Intermittent fasting (work towards target 2 - 8pm eating window)
- Supplemented with Exogenous ketones (Caprilic acid and BHB salts during fasting window and can also be consumed during eating window)
- (2) Repurposed drugs cocktail per Care Oncology Clinic (submitted info, waiting for treatment plan)
- (3) Supplements
Subscribe to:
Posts (Atom)
